The emergence of resynchronization therapy has led to an increase in attempts at left ventricular lead placement via the coronary sinus (CS). The MIRACLE study program [LEO05] reported a 91.6% success rate for LV lead placement, while COMPANION [BRI04] revealed an 89% success rate for LV lead placement. Another report indicated a similar 92% success rate with LV lead placement. [DIV08] Though we counsel our patients on a LV lead placement success rate at 88-92%, our center demonstrated a 97% success rate (64 of 66 patients) with LV lead placement within the range from 2:30 to 5:30 o’clock in the left anterior oblique (LAO) view. [WIL10]
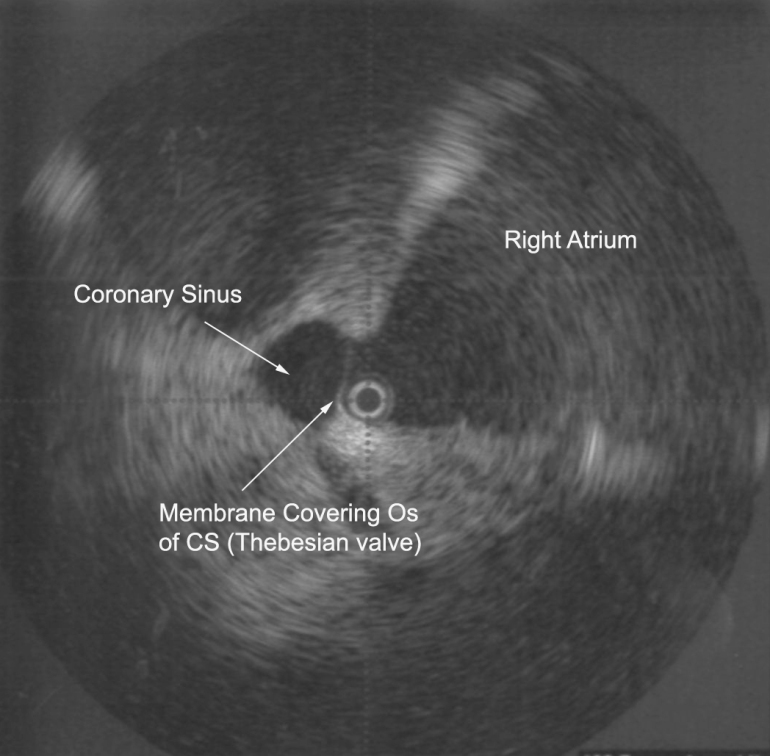
There are many reasons for difficult CS access including Thebesian valves, cardiac vein ostial valves, and Chiari networks. The image shown below is representative of the ostial valve of the coronary sinus (aka, Thebesian valve) that prevents engagement of the CS and ultimately precludes LV lead placement. Routine attempts at engaging the coronary sinus with deflectable EP catheters as well as hydrophilic guide wires were met without success. A 9MHz radial intracardiac echo (ICE) probe (UltraICE, Boston Scientific Corp) was introduced via a steerable sheath (Agilis, St. Jude Medical) to evaluate the CS anatomy. This image demonstrates a Thebesian valve covering the entire CS osmium with no obvious accessible fenestration or defect. LV lead placement was aborted and patient was referred for epicardial LV lead placement via cardiothoracic surgery.
Prior reviews of CS anatomy (PEJ08) revealed the presence of Thebesian valves in 80% of cases and Chiari networks were found in 10% of cases. It covered one-fifth in 7%, one-third the os in 29%, one-half in 27%, two-thirds in 14%, and the entire os in 5%. The average diameter of the CS os was 8mm with a range of 3-15mm. Appreciation for the anatomic variations of the normal human CS as well as experience with ICE may help reduce complications and improve success of LV lead implantation.
References:
LEO05 Leon AR, Abraham WT, Curtis AB, et al.; for the MIRACLE Study Program, “Safety of Transvenous Cardiac Resynchronization System Implantation in Patients with Chronic Heart Failure: Combined Results of Over 2000 Patients from a Multicenter Study Program,” J Am Coll Cardiol, 2005;46(12):2348–56.
BRI04 Bristow MR, Saxon LA, Boehmer J, et al., “Cardiac-Resynchronization Therapy with or without an Implantable Defibrillator in Advanced Chronic Heart Failure for the Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Investigators,” N Engl J Med, 2004;350(21):2140–50.
DIV08 D’Ivernois C, Lesage J, Blanc P, “Where are left ventricular leads really implanted? A study of 90 consecutive patients,” Pacing Clin Electrophysiol, 2008;31(5):554–9.
WIL10 Williams JL, Lugg D, Gray R, Hollis D, Stoner M, Stevenson R, “Patient Demographics, Complications, and Hospital Utilization in 250 Consecutive Device Implants of a New Community Hospital Electrophysiology Program,” American Heart Hospital Journal, V. 8, No. 1 (Summer, 2010), pp. 33-39.
PEJ08 Pejkovic B, Krajnc I, Anderhuber F, Kosutic D, “Anatomical Variations of the Coronary Sinus Ostium Area of the Human Heart,” J Int Med Research, V. 36 (2008), pp. 314-321.