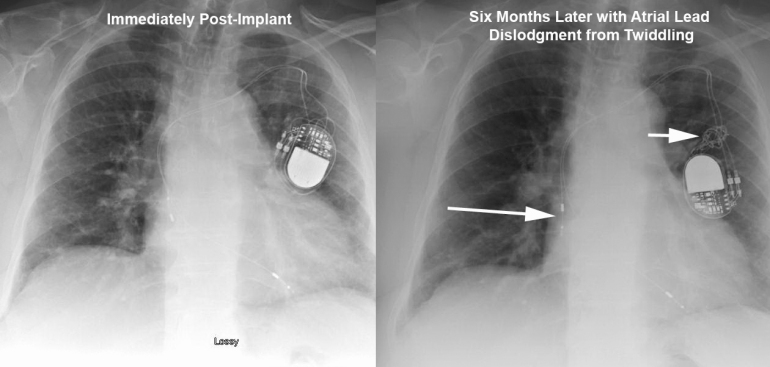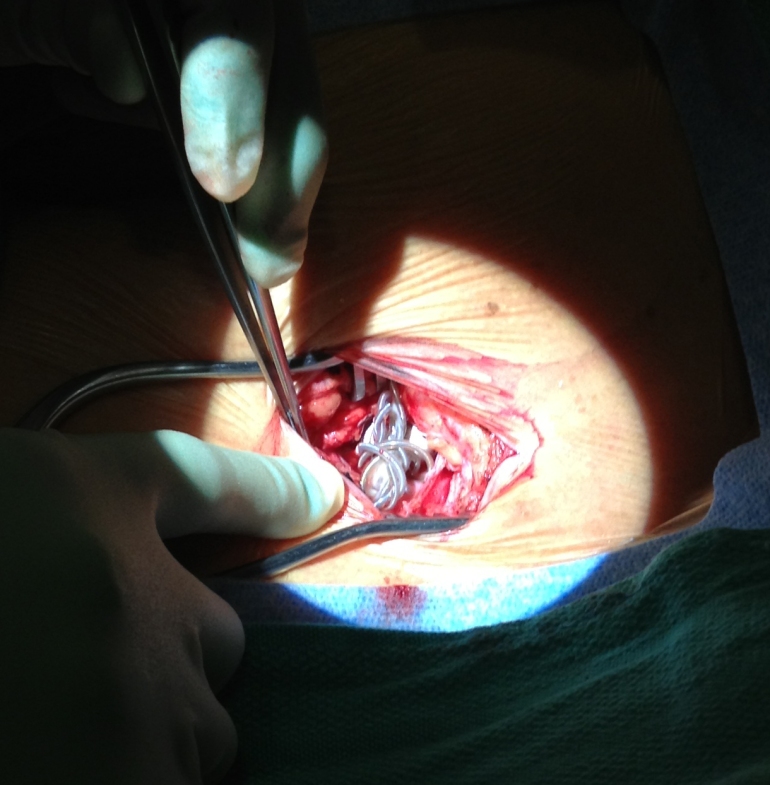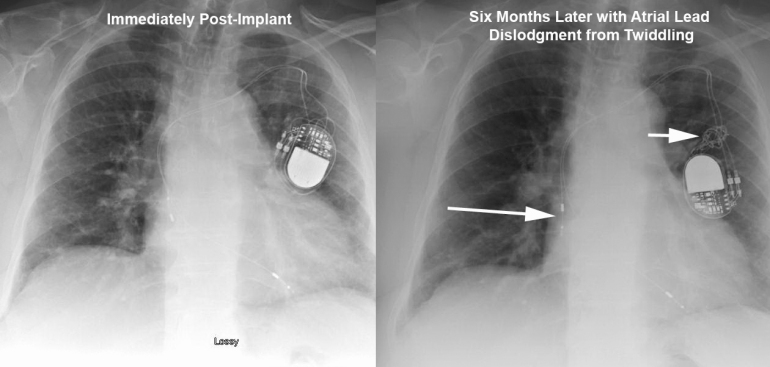
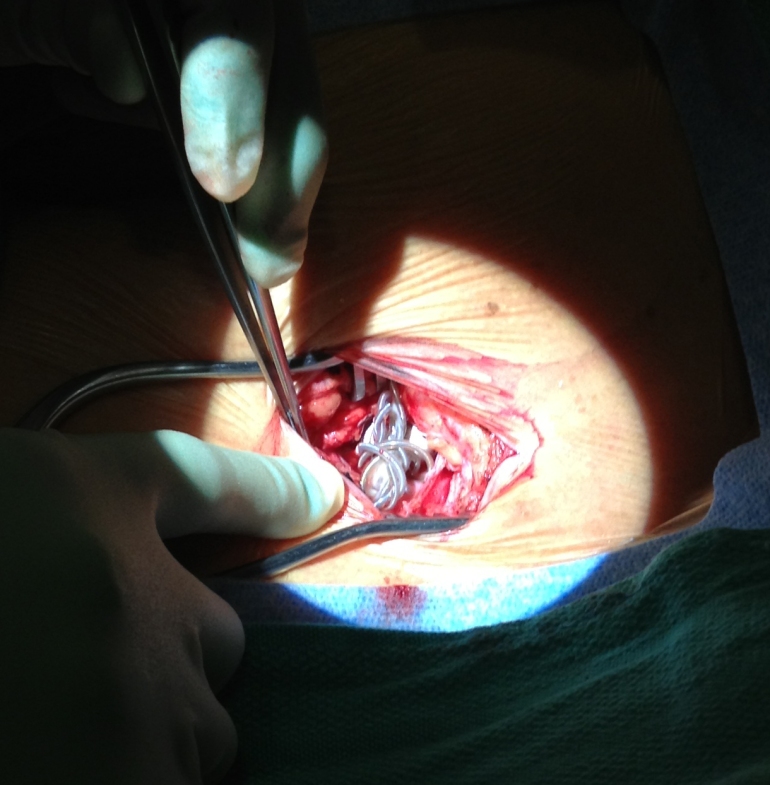
This elderly patient presented 6months after a dual chamber pacemaker was implanted due to symptomatic chronotropic incompetence. They reported recurrence of exertional shortness of breath that was experienced before pacemaker implantation. Device interrogation revealed complete loss of capture in the atrial lead. The top Figure depicts lead orientation before (left) and after (right) patient twiddling resulted in loss of slack in both leads with frank atrial lead dislodgement. Arrows show the dislodged atrial lead and knotted leads. The bottom Figure shows the intraoperative finding of knotted leads in the pocket. The leads were carefully unknotted, stylets placed, and leads repositioned with normal parameters. Originally described in 1968 [1], twiddling refers to patient manipulation of pacemaker can or leads that may lead to malfunction. It has a reported incidence of 0.07% in a series of 17000 patients. [2] The patient underwent an uneventful lead revision by repositioning the atrial lead and adding slack to the ventricular lead.
1 Bayliss CE, Beanlands DS, Baird RJ, “The pacemaker-twiddler’s syndrome: a new complication of implantable transvenous pacemakers,” Can Med Assoc J, V. 99 (1968), pp. 371–3.
2 T. Fahraeus and C. J. Hoijer, “Early pacemaker twiddler syndrome,” Europace, Vol. 5 (July 2003), pp. 279-281.
Published by Heart Rhythm Center
Dr. Williams obtained his undergraduate degree with a double major in Biomedical and Electrical Engineering at Vanderbilt University. He was then awarded a Keck Fellowship for graduate school at the University of Pittsburgh where he obtained his Master’s degree in Bioengineering.
Dr. Williams went on to obtain his medical degree at Drexel University in Philadelphia and completed 5 years of Fellowship training in both Cardiovascular Diseases and Clinical Cardiac Electrophysiology at the University of Pittsburgh Medical Center.
His unique background and extensive knowledge of both engineering and cardiology have earned Dr. Williams many accolades in both clinical and academic settings. He’s published over 20 manuscripts and abstracts in the field of cardiology/electrophysiology and has received awards from both the American College of Cardiology Foundation and the National Institutes of Health.
Dr. Williams started in the Invasive Electrophysiology Laboratory at The Good Samaritan Hospital in 2008 and the Heart Rhythm Center published outcomes on pacemaker and defibrillator implantations as well as the safety and efficacy of high frequency jet ventilation during EP studies with ablation under his direction. He is Chair of the Quality Committee at the Florida Chapter of the American College of Cardiology.
View all posts by Heart Rhythm Center